Overview: The United States Preventive Services Task Force (USPSTF) recommended recently against screening asymptomatic patients for thyroid cancer. The guidelines, published in the Journal of the American Medical Association, at first glance may appear counter-intuitive. However, they underscore the growing recognition of the problem of overtreatment in thyroid cancer diagnosis. “As physicians guided by the principle of ‘first, do no harm,’ we should be relieved that the USPSTF reached this conclusion,” state Louise Davies, M.D. and Luc G. T. Morris, M.D. in a JAMA Otolaryngology – Head & Neck Surgery editorial.
The USPSTF Recommendations: The USPSTF recommended against screening asymptomatic patients for thyroid cancer using neck palpations or ultrasound – giving the practice a D grade. This means the group believes there is no net benefit or that the harms outweigh the benefits. The recommendations do not apply to individuals with clinical symptoms or who have increased risk of thyroid cancer due to environmental or genetic factors.
The Rationale Against Screening: The task force noted that the incidence of thyroid cancer detection in the U.S. has increased by 4.5% per year over the last 10 years, faster than for any other cancer, but the mortality rate remained unchanged. This suggests that increased detection is not saving lives, but rather, is finding more cases of small, papillary thyroid cancers (PTC) that are unlikely to grow or progress. The USPSTF found that in such PTC cases, there is no evidence that treatment of asymptomatic patients was associated with better outcomes than the treatment of symptomatic patients – or even that treatment of asymptomatic screening-detected cases was better than no treatment.
Potential Harms of Screening and Treatment: In their editorial, Drs. Davies and Morris note that thyroid cancer is a low-mortality disease, with approximately 1,600 deaths in the U.S. each year. In comparison, screening would identify approximately 250 million people with thyroid nodules who would undergo additional diagnostic tests and invasive procedures, and who would experience the anxiety of a potential cancer diagnosis. They also point out that the risks of thyroid surgery, which – while small – would become much greater when scaled to a large population through screening. Thyroid surgery risks include:
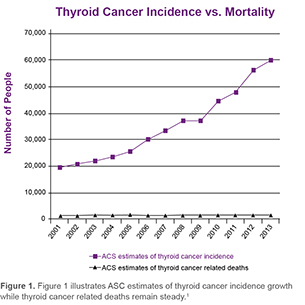
Figure 1. illustrates ASC estimates of thyroid cancer incidence growth while thyroid cancer related deaths remain steady.